Guillain-Barre Syndrome (GBS), an acute autoimmune neuropathy that can follow infection, vaccination, and surgery, can also lead to the development of scoliosis in some cases. Though it is unknown why scoliosis develops secondarily to GBS, there have been several cases reported in the literature going back to the 1950s. To date, every published case of scoliosis secondary to GBS has been treated surgically with a spinal fusion procedure. However, orthopedic surgeons at NewYork-Presbyterian and Columbia recently treated a six-year-old with kyphoscoliosis secondary to GBS.
Below, Benjamin D. Roye, MD, MPH, a pediatric orthopedic surgeon at NewYork-Presbyterian and Columbia, discusses the details of their recent case, their approach to management, and how it could potentially change the approach to managing scoliosis associated with GBS.
How the Patient Presented
The patient, a 6-year-old, was initially treated at an outside hospital for neurological symptoms accompanying a COVID-19 infection. After receiving a lumbar puncture and an MRI scan, they were diagnosed with the Miller Fisher variant of GBS based on the presence of ophthalmoplegia, ataxia, and areflexia. They were discharged and readmitted to the hospital three months later when their symptoms recurred with a metapneumovirus infection. Their symptoms resolved after a few days, and they were discharged home again. About five months after their second hospital discharge, they were referred to our outpatient orthopedic clinic by their physical therapist for an evaluation for possible scoliosis.
Making the Diagnosis
During the physical exam, we didn’t find any obvious neurological deficits and there was no paraspinal prominence on the forward bend test. However, their X-ray showed a 15-degree coronal Cobb angle and 65-degrees of kyphosis. Since their coronal curve was under 20 degrees, we opted to treat them conservatively, holding off on bracing and continuing physical therapy.
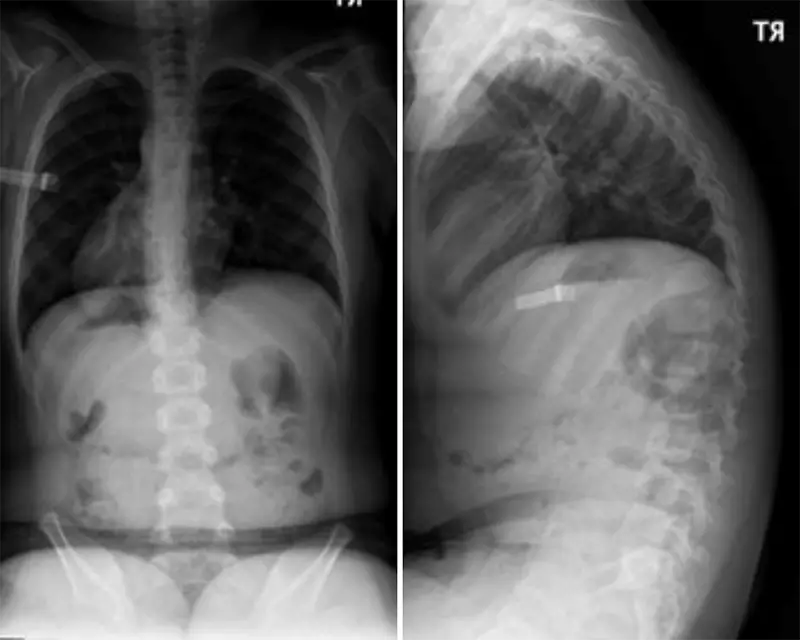
X-rays showing a left thoracic coronal curve of 13° and kyphosis of 77°.
We evaluated them again at seven months and found that their coronal curve was stable at 13 degrees, but their kyphosis had increased to 77 degrees. We continued with physical therapy, focusing on their trunk alignment, and monitored their progress. At one year, their kyphoscoliosis had remarkably corrected, with their coronal curve completely resolved and their kyphosis normalized at 38 degrees. They are doing well today; at their last follow up, they were walking well and had normal spinal alignment.
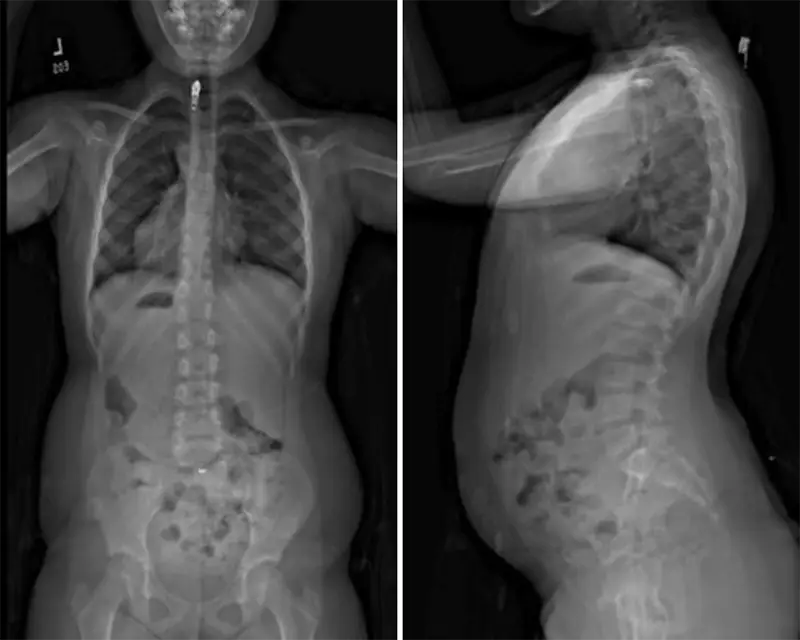
Repeat x-rays the one-year post index visit show the coronal curve completely resolved and kyphosis of 38° was measured.
Spontaneous Resolution without Surgical Intervention
To our knowledge, this is the first published report of scoliosis secondary to GBS that resolved spontaneously without surgery. We managed the patient conservatively, foregoing bracing and surgery in favor of continued physical therapy. While we don’t know for sure why their curvature resolved, it’s likely that the physical therapy was helpful and played a role. When looking at published cases of scoliosis secondary to GBS, our case does have some notable differences. Our patient’s spinal curve was less pronounced than other cases and they were referred for orthopedic treatment in a matter of months rather than years. Their early diagnosis and treatment with physical therapy may have prevented the need for surgery in the future.
Lessons Learned
While this is just one case, it demonstrates that conservative management can be successful and that not all cases of kyphoscoliosis associated with GBS will continue to worsen over time without surgery. This suggests that orthopedists who are managing spinal alignment problems in children to strongly consider options that could avoid surgery, including physical therapy to bracing. Not every case of scoliosis will progress to become worse, and the potential to avoid surgery has a huge benefit for our patients.



