About 1 in 8 men will be diagnosed with prostate cancer in his lifetime, while 1 in 44 will die of it, according to the American Cancer Society. Prostate cancer is highly treatable if detected early, which makes testing all the more imperative. But while more than 3 million prostate biopsies are performed annually, the prevailing technique, known as the transrectal biopsy, exposes patients to the risk of infection.
The transperineal biopsy is an alternative approach with fewer complications, but it has yet to be widely adopted as the new standard for prostate biopsies because high-level evidence supporting its benefits has been lacking.
Jim C. Hu, MD, MPH, a urologic oncologist and director of LeFrak Center for Robotic Surgery at NewYork-Presbyterian and Weill Cornell Medicine, recently led a trial comparing the transrectal and the transperineal approaches to assess their ability to accurately diagnose prostate malignancies while minimizing post-biopsy infections.
The results of this pivotal study were recently published in JAMA Oncology. Below, Dr. Hu discusses the findings and how they will impact patient care moving forward.
Why does the transrectal biopsy pose the risk of infection for patients?
The transrectal biopsy is considered a contaminated procedure because the biopsy needle passes through the rectum. To avoid the development of post-biopsy infection, our patients have to perform an enema prior to the procedure and take prophylactic antibiotics. Despite these safety precautions, we observe instances of complicated and uncomplicated post-biopsy genitourinary infections and urosepsis after 5-7% of transrectal biopsy. For those who don’t develop an infection, we are exposing them to additional antibiotic use, which can contribute to the development of antibiotic resistance in the future.
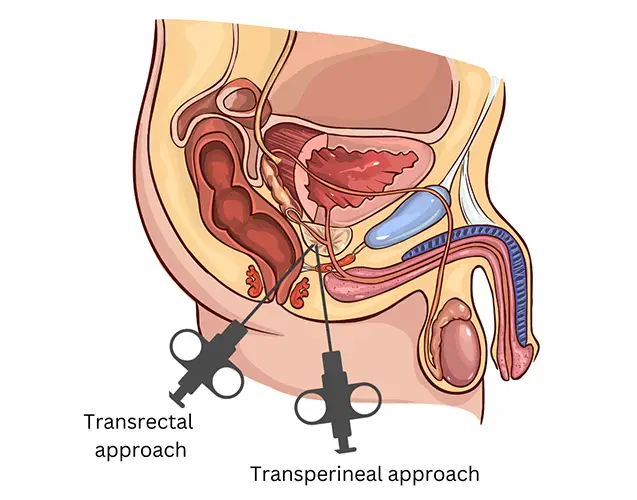
During a transperineal biopsy, the physician inserts the biopsy needle through the skin of the perineum directly into the prostate, thus eliminating the patient’s exposure to rectal bacteria and lowering the risk for infection that they are susceptible to through the transrectal approach.
But for decades, transrectal biopsy has been the only method of prostate biopsy that urologists in the United States knew how to do. There has been no strong evidence or pressure for that to change. So, despite the risk of infectious complications, we continued to perform this procedure on our patients.
How does the transperineal approach differ and why did you want to test it?
Transperineal biopsy involves inserting the biopsy needle through the skin of the perineum into the prostate, thus eliminating the patient’s exposure to rectal bacteria and lowering risk for infection. Transperineal biopsy was traditionally performed under general anesthesia, but in the past few years, the technique became more refined and the technology more advanced. I hypothesized that the transperineal approach would have a lower infection rate and a diagnostic accuracy similar to transrectal biopsy.
How did you test your hypothesis?
We tested my hypothesis in a 10-center, randomized controlled trial, where we randomized participants with suspicion for prostate cancer to receive either transperineal biopsy without antibiotic prophylaxis, or a transrectal biopsy with targeted prophylaxis, rectal culture screening for fluoroquinolone-resistant bacteria, and antibiotic targeting to the culture and sensitivity results. Both procedures were performed in office using local anesthesia.
We enrolled 875 participants from February 2021 through March 2024, with 382 in the transperineal arm and 370 in the transrectal arm. Our results confirmed my initial hypothesis — there were no post-biopsy infections in the transperineal group, whereas there were six (1.6%) transrectal biopsy infections. Additionally, we detected high grade cancer in 55% of the transperineal biopsies vs. 52% of the transrectal.
For the first time, we now have strong evidence showing the benefits of the transperineal approach over the transrectal. I expect that more urologists, with this data, will become interested in adapting the transperineal approach and offering it to patients. My hope is that it will eventually become the standard of care.
— Dr. Jim Hu
How do you think this research can support a change in clinical practice?
For the first time, we now have strong evidence showing the benefits of the transperineal approach over the transrectal. Men undergoing a prostate biopsy don’t need to risk getting an infection while going through one of the most commonly performed diagnostic tests to rule out cancer. And while the transperineal biopsy was performed previously under sedation or general anesthesia, our study shows that it can be successfully done in office using local anesthesia, making it generalizable to the three million men who annually who get prostate biopsies world-wide. I expect that more urologists, with this data, will become interested in adapting the transperineal approach and offering it to patients. My hope is that it will eventually become the standard of care.



