About 80% of patients who require pacemakers, particularly those with sinus node dysfunction or heart block, need a device that uses leads to connect to both the right atrium and the right ventricle to keep atrial and ventricular pacing in sync.
Last year, a research study coauthored by James E. Ip, MD, FACC, FHRS, director of cardiac pacing and implantable devices at New York-Presbyterian and Weill Cornell Medicine, established the efficacy and safety of a dual-chamber leadless pacemaker system. As part of that trial, Dr. Ip and his colleagues at New York-Presbyterian and Weill Cornell Medicine were the first center in New York and the second center in the U.S. to implant this novel pacemaker in a human subject.
More recently, new data has been published in Circulation from the multicenter, international clinical trial that supports the device’s reliability, showing that it achieves atrioventricular (AV) synchrony 98% of the time. Below, Dr. Ip discusses the latest findings from the trial and the implications for clinical care.
Research Background
AV synchrony occurs when the contractions of the atrium and ventricle are synchronized. When a person’s heart is working normally, their heartbeat should proceed from top to bottom in a sequential fashion. This is essential for proper heart function and adequate cardiac output. However, in some patients, that sequence is disrupted because of different heart conditions, medications, and aging.
Wired pacemakers have been used for decades as one way to maintain AV synchrony. Since they are physically connected, the communication between the pieces is seamless. However, there are many downsides to those devices, including the potential for lead fractures and development of infection.
Single-chamber leadless pacemakers have been around for the last decade; however, they only pace the ventricle and do not support consistent AV synchrony. We have been looking at dual-chamber devices to see if they can achieve the effect of wired pacemakers in both the right ventricle and the right atrium. This requires placement of two capsule-sized devices that must communicate with each other wirelessly to ensure AV synchrony.
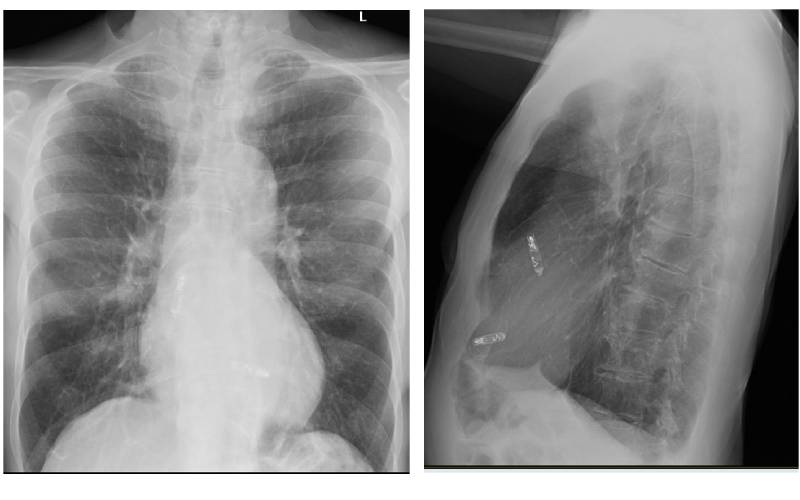
A chest X-ray from a patient who had a dual chamber leadless pacemaker implanted.
Research Methods
We conducted a prospective, multicenter, international study looking at the outcomes of patients who were implanted with the novel dual-chamber leadless pacemaker system. Last year, we published the initial results of the first 300 patients in the study in the New England Journal of Medicine, showing the safety and efficacy of the device and leading to its FDA approval and coverage through Medicare.
In our current study, we evaluated 384 patients who had the dual-chamber leadless pacemaker using an external electrocardiogram (ECG) recording device that they wore temporarily. The recordings were used to measure AV synchrony as the patients were in various positions (laying on their backs and sides, sitting, and standing) and when they walked slowly and quickly. We also assessed the impact of various heart rates, especially faster heart rates, on AV synchrony.
Study Findings
Using a standard definition of AV synchrony with a 300-millisecond limit, we showed that the dual-chamber system achieved a mean AV synchrony of 98% of beats across all postures. But since the normal interval between the top and bottom chambers of the heart is much shorter than that, we also tested the pacemaker system with a stricter, standard definition of AV synchrony that is based on the patient-specific AV delays programmed for each device.
Under this stricter definition, the device still provided excellent coordination, with mean AV synchrony of 96.3% of beats across a variety of postures, activities, and heart rates. Since wearing an external ECG recording device is cumbersome for patients, we also analyzed the AV synchrony report produced by the device itself and found that it was comparable to our external validation. If anything, it underestimated the true performance of the device. That means clinicians can feel comfortable looking at that device-generated data to be sure the pacemaker is providing AV synchrony.
Clinical Implications
Since we published our research last year on the effectiveness of the dual-chamber leadless pacemaker, there has been a significant increase in patients who have been able to access the technology. The small and wireless design means fewer complications and infections, along with greater comfort. There are some potential downsides, such as shorter battery life compared with a traditional pacemaker, but we hope to see that improve over time as new versions are developed. Choosing which pacemaker is right for a patient requires a nuanced discussion with them, but it is wonderful to have additional options.
We are continuing to follow these patients as well as newer patients who are receiving the dual-chamber leadless pacemaker to see how these devices perform over time and how the implants communicate with each other. Going forward, we will need to figure out which patients are best positioned to benefit from this new technology. But it is safe to say that today that we have a viable, safe, and effective alternative to conventional pacemakers.