According to recent research, atrial fibrillation (AFib) affects one out of every 20 adults in the United States. The field of electrophysiology has made great strides in the past two decades when radiofrequency thermal ablation was first introduced to treat AFib. A novel, largely non-thermal cardiac ablation technology – pulsed field ablation – has the potential to further expand the application of these procedures.
Christopher F. Liu, MD, medical director of cardiac electrophysiology services at NewYork-Presbyterian and Weill Cornell Medicine, recently collaborated with colleagues from 30 centers across the country in the AdmIRE (Assessment of Safety and Effectiveness in Treatment Management of Atrial Fibrillation With the BWI IRE Ablation System) study to assess the long-term safety and effectiveness of this new technology for the treatment of AFib.
Below, Dr. Liu, a pioneer in complex arrhythmia ablation and structural heart electrophysiology, discusses the study’s findings and implications for the treatment of AFib going forward.
Evolution of Cardiac Ablation Techniques
Ablation performed for AFib began with thermal ablation to destroy the electrical cells of the heart that go rogue. Historically, radiofrequency energy has allowed us to use an electrical current to cauterize the tissues in the heart responsible for interrupting its normal rhythm. That worked reasonably well, but in its earlier iterations the thermal energy couldn’t be confined to just the heart tissue and the surrounding structures, such as the esophagus and phrenic nerves, were at risk of injury. As rare as these complications were, when they did happen, patients could be devastated by stroke or death. However, with advances in our understanding of anatomy and in the technology and delivery techniques, thermal ablation has evolved into a very successful tool. Now, thermal probes allow us to measure how much we were heating the esophagus and we developed ways to localize the phrenic nerves to avoid causing collateral damage.
Pulsed field ablation (PFA) predates thermal ablation. However, it was initially unsuccessful because the electrical energy delivered could not be controlled, resulting in unpredictable areas of ablation effect. This changed in 2020, when scientists and electrophysiologists began using animal models to design catheters and waveforms that could be miniaturized to deliver more precise electrical pulses that would still be therapeutic and can be targeted much more precisely. When you use PFA now, the electrical shocks tend to be more selective for cardiac tissue and less subject to causing damage to the esophagus and the phrenic nerves.
The AdmIRE Study
Through the AdmIRE study, we sought to determine if PFA measures up to traditional thermal ablation for paroxysmal AFib, both in safety profile and long-term efficacy. This PFA system uses a novel variable-loop catheter integrated with an electroanatomic mapping system. This allows us to use real-time non-fluoroscopic procedural guidance in ablating the lesions in the heart, and that's very powerful. In treating AFib, thermal ablation energy is typically delivered to fairly extensive areas of the heart by moving from spot to spot to spot – a procedure that can be tedious and time-consuming. With PFA, we are able to deliver pulsed energy more efficiently to a larger area in one fell swoop as opposed to the point-by-point delivery.
The results from this study showed overall excellent clinical outcomes that were as successful as what we have been able to achieve with radiofrequency ablation.
— Dr. Christopher Liu
Study Results and Future Implications
Our multicenter study involved 277 patients with drug-refractory symptomatic paroxysmal AFib who underwent pulmonary vein isolation using the PFA catheter with a compatible electroanatomic mapping system. The results from this study showed overall excellent clinical outcomes that were as successful as what we have been able to achieve with radiofrequency ablation. Compared to thermal ablation, the tissue-selective mechanism of PFA should reduce the risk of collateral tissue injury and the 3D mapping integration minimized the use of fluoroscopy.
These results are very promising in a number of ways. We now feel more comfortable offering PFA to older people with comorbid conditions because it is more straightforward, simpler, and potentially safer for patients presenting with more complicated health issues. For thermal ablation, we typically use general anesthesia. With PFA, we have started to do more procedures with conscious or deep sedation. We expect PFA to take even less time going forward and it is already allowing us to perform more procedures per day.
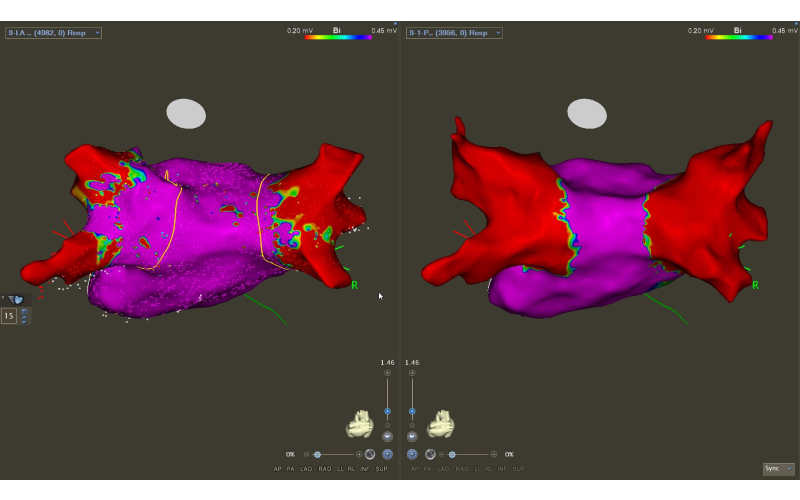
Left atrium electrical activity before and after pulmonary vein ablation (red = electrically quiet).
PFA does have some limitations in certain areas of the heart, so thermal ablation still definitely has a role. We are looking forward to partnering with scientists and industry to develop catheters that can deliver either type of ablation energy, and that will give us the maximum flexibility to treat every possible patient.
PFA also opens up the possibility for treating AFib and performing a left atrial appendage closure during the same procedure because it is less likely to cause swelling or alter the anatomy. Theoretically, we could address all the concerns about AFib at the same time – the arrhythmia and the associated risk of stroke.
We already were very comfortable using thermal ablation, and many of us originally questioned whether we need the PFA approach. However, with experience using these new systems, many of us have now been turned into believers. As PFA technology continues to advance, it may become the new standard of care for many patients with AFib.



