A NewYork-Presbyterian/

David A. Gudis, MD
The Orbital Resection By Intranasal Technique (ORBIT) system was developed to help predict surgical outcomes for all primary benign orbital tumors, aiding surgical planning and improving communication with patients. The ORBIT system was validated in a study published in the International Forum of Allergy & Rhinology.
“Every benign or malignant tumor in the body should have some common language with which doctors and patients can communicate about diagnostics, the implications of intervening or not intervening, the best surgical approach, and the possible outcomes,” says David A. Gudis, MD, chief of rhinology and anterior skull base surgery in the department of otolaryngology- head and neck surgery at NewYork-Presbyterian/
In my mind, the most important thing to come out of this collaborative study with colleagues around the world is that we can communicate honestly and with an informed perspective to patients regarding their risks and alternative treatment options.
— Dr. David A. Gudis
It has been about 30 years since the development of endoscopic nasal and sinus surgery, followed a decade later by endoscopic skull-based surgery. However, it has only been in the last 10 years that surgeons have begun to utilize endoscopic endonasal orbital surgery for resection of well-encapsulated tumors that would otherwise require an external approach to the eye. The technique involves inserting the endoscope through the nostrils and accessing the eye socket through the outer walls of the sinuses, Dr. Gudis explains.
The endoscopic endonasal orbital approach is not right for every type of orbital tumor. The decision to use that approach is based on an array of factors including the anatomical structures at risk and the potential for complications. “A 1 cm tumor sitting right up against the medial wall of the eye socket is going to be a very different surgery from a 3 cm tumor that is sitting lateral to the optic nerve. The idea is, before we can start talking about interventions and outcomes for patients, we need to speak about these lesions with a common language,” Dr. Gudis says.
With the growing use of this technique, there was a push to develop standardized language to classify tumors and help determine the surgical approach. In 2019, an international panel of experts across disciplines developed the Cavernous Hemangioma Exclusively Endonasal Resection (CHEER) system as an anatomic-based classification framework. The CHEER system, which uses stages I-Vb, has been the gold standard. However, results from a systematic review found similar surgical outcomes between orbital cavernous hemangiomas and other primary benign orbital tumors when an endoscopic endonasal approach was used, pointing to the need for a more broad-based classification system that includes other tumors, such as solitary fibrous tumors and schwannomas.
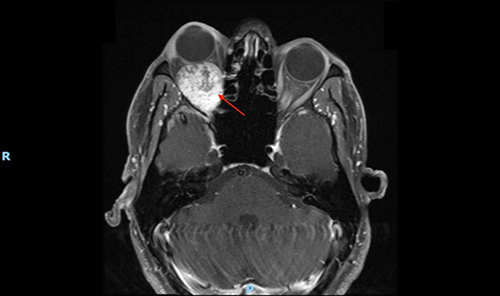
Benign right orbital tumor, pushing the eye forward
(Photo courtesy of Dr. Gudis)
“The CHEER staging system was a way to communicate specifically about cavernous hemangiomas. But this new staging system, called the ORBIT staging system, is a simpler classification system and can be applied to other benign tumors as well,” Dr. Gudis says.
The ORBIT classification system, which is adapted from the CHEER framework, uses CT and MRI imaging to determine the location of the tumor, looking specifically at the epicenter of the tumor and its greatest extension. Class I tumors, the lowest risk classification, are extraconal, meaning they are outside of the muscles in the eye socket. The ORBIT system goes up to class V tumors, which can be extraconal or intraconal but have intracranial extension through the superior orbital fissure, indicating that they are the most complicated and highest risk. At a higher classification it might be necessary to forego an endoscopic technique or to combine it with another approach, Dr. Gudis says.
The five-class ORBIT staging system describes the anatomical location of the tumor epicenter:
- Class I: Extraconal
- Class II: Intraconal; anterior to the intersection of the ophthalmic artery and optic nerve
- Class III: Intraconal; posterior to the intersection of the ophthalmic artery and optic nerve
- Class IV: Extraconal or intraconal; extension into the pterygopalatine and/or infratemporal fossae through the inferior orbital fissure
- Class V: Extraconal or intraconal; intracranial extension through the superior orbital fissure
To validate the new system, the researchers retrospectively assigned an ORBIT class to primary benign orbital tumors from 110 patients across 11 international centers of excellence, including NewYork-Presbyterian/
The CHEER staging system was a way to communicate specifically about cavernous hemangiomas. But this new staging system, called the ORBIT staging system, is a simpler classification system and can be applied to other benign tumors as well.
— Dr. David A. Gudis
Overall, the analysis showed a trend toward higher-class lesions being associated with a greater risk for incomplete resection. Gross total resection was achieved in approximately 88% of class I ORBIT tumors, compared with 60% of class V tumors, though the difference did not achieve statistical significance.
Additionally, the analysis demonstrated that an endoscopic endonasal orbital approach for the resection of primary benign orbital tumors is generally effective and has a low rate of adverse events. Worsening of vision, diplopia, and recurrence were low across ORBIT stages.
The ORBIT staging system is already being adopted and will be beneficial both in clinical care and for research purposes, Dr. Gudis says. In particular, the common language created by the classification system allows surgeons to counsel patients about potential surgical outcomes.
“If I have study that collects 1,000 cavernous hemangiomas that were removed endoscopically through the nose around the world and 5 of those patients lost vision, those data are critical. But if every one of those 5 patients had an ORBIT stage 5 tumor, and the patient in front of me has an ORBIT stage 2 tumor, I can feel more comfortable reassuring that patient that the risk for his or her particular lesion is very low. Conversely, if that patient does in fact have an ORBIT stage 5 tumor, then they need to be counseled that the risk is much higher,” Dr. Gudis says.
The staging system is also essential for surgical planning, he says, providing valuable information about the safety of various approaches, as well as how many surgeons are needed and what types of equipment should be available in the surgical suite. On the research side, primary benign orbital tumor surgeries are still uncommon so the tumor staging will be important as more outcomes data is collected and analyzed.


