In the Weill Cornell Medicine Sean Parker Institute for the Voice, Babak Sadoughi, MD, and Anaïs Rameau, MD, MPhil, laryngologists with the Department of Otolaryngology – Head and Neck Surgery at NewYork-Presbyterian/
Dr. Babak Sadoughi
Dr. Anaïs Rameau
Vocal Fold Paralysis: Evaluating the Role of Injection Laryngoplasty
Unilateral vocal fold paralysis, which presents with dysphonia, shortness of breath, and difficulty swallowing, results from damage to the recurrent laryngeal nerve generally due to cancers, trauma, or surgery. Swallowing dysfunction is particularly concerning for its risk of aspiration leading to pneumonia and the need for enteral feeding in the immediate postoperative setting. Injection laryngoplasty has become a key component in treatment as a temporary delaying measure and to help improve glottic closure, airway protection, and cough efficiency.
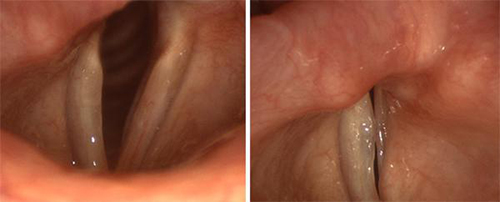
The vocal folds on the left of both images above are paralyzed. Even with extreme effort, they cannot meet their opposing partners.
While injection can improve voice outcomes after paralysis, there is limited information about its potential efficacy in decreasing aspiration. According to Dr. Babak Sadoughi, the indication of injection for aspiration management in iatrogenic unilateral vocal fold paralysis currently relies on anecdotal evidence and empirical practice and thus prompted him to conduct a review of the literature to guide best practice. In a study published in the April 2022 issue of The Laryngoscope, Dr. Sadoughi sought to determine whether patients with iatrogenic vocal fold paralysis who undergo injection laryngoplasty have improved aspiration outcomes and diet advancement in the early postoperative setting.
The initial in-depth search on several databases yielded 1,590 articles; of that number 92 articles underwent full review by the Weill Cornell Medicine investigators. The final qualitative review consisted of 14 case series studies comprising 582 patients with a total of 348 patients treated with injection laryngoplasty for unilateral vocal fold paralysis.
The researchers concluded that the evidence in the literature to support injection laryngoplasty to reduce the risk of aspiration in the acute setting of iatrogenic unilateral vocal fold paralysis was inconclusive. They further note that the indication of injection laryngoplasty for aspiration management continues to rely on empirical practice without validation against control subjects. What is needed are prospective investigations with validated, objective measures to definitively demonstrate the effectiveness of injection laryngoplasty for that indication, as well as support guidelines for timing of interventions.
Machine Learning Enhances Diagnostic Capabilities
Dr. Anaïs Rameau has developed a particular expertise in the use of artificial intelligence (AI) in the diagnostic streamlining of laryngological and swallowing disorders and the application of AI to video laryngoscopy.
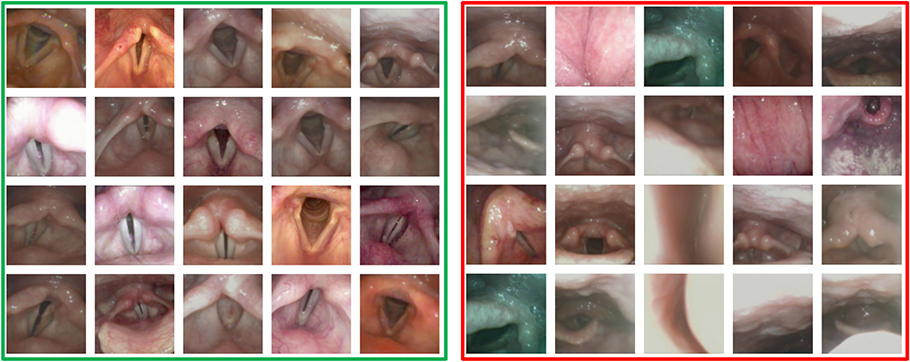
“Laryngologists capture a large number of videos of the larynx and the vocal folds, but there are certain challenges that come with these videos,” says Dr. Rameau. “First, the videos are not static images, unlike radiology or pathology. We have many frames and not all the frames are useful for diagnostics. Another challenge is that the camera is always mobile, thereby not allowing a standard perspective on the structures of the larynx. So, we've been tackling how to extract only those frames that have diagnostic value. With a grant from the American Laryngological Association, over the past year we have developed an algorithm that is able to recognize informative frames among the large number of laryngoscopy videos, basically automating this process, obtaining a precision rate for the recognition of informative frames that is above 80 percent.”
Dr. Rameau has applied the automated algorithm to recognize images of the larynx in patients who have a normal layer and in patients who have a polyp. “We then used this mechanism to recognize the presence of the polyp and again our precision was above 80 percent,” she says. “We’ve been able to not only automate the recognition of informative frames, but we are also currently automating the recognition of abnormal lesions on the vocal fold.”
Informative laryngeal frames (left) versus uninformative laryngeal frames (right)
“We’re limited by the number of patients with polyps who come to our center, which does not represent its prevalence across the country,” notes Dr. Rameau, who is collaborating with colleagues in the Department of Otolaryngology – Head and Neck Surgery at NewYork-Presbyterian/
In other AI projects, Dr. Rameau and colleagues at the Weill Cornell Medicine Sean Parker Institute for the Voice recently conducted a scoping review for studies on AI and office laryngoscopy in five databases focused on vocal fold vibration analysis, lesion recognition, and vocal fold movement determination. The most frequently automated tasks were recognition of vocal fold nodules, polyp, paralysis, paresis, and cyst. Imaging modalities included high-speed laryngeal videos, stroboscopy, and narrow band imaging endoscopy.
The authors recommended that greater interdisciplinary collaboration among science, technology, engineering, and math (STEM) specialists and otolaryngology research teams can lead to improved demographic reporting and larger and more geographically diverse datasets, which will be critical to future research on AI in office laryngoscopy.
Expanding Access to Specialized Laryngological Care
According to Dr. Rameau, the relatively few number of laryngologists in the United States tends to practice in urban areas, limiting access to this highly specialized field in other parts of the country and indeed the world. “A recurring theme in my research is to try to make some of the high-end subspecialized care available to all.”
To that end, Dr. Rameau and her Weill Cornell Medicine colleagues conducted a scoping review to outline disparities research within laryngology and identify gaps in knowledge and guide future research. Of the nearly 5,000 abstracts identified, 51 articles were ultimately included. The most frequently examined condition in relation to disparities was laryngeal cancer, followed by voice disorders, deglutitive disorders, and airway disorders. Sources of inequity ranging from the most common to least common were race/ethnicity, sex/gender, insurance status, geography, income, and education level. No study examined the association of LGBTQ identity with inequity. The researchers concluded that the limited extent of disparities research in laryngology requires further investigation. Results were published in the February 2022 issue of The Laryngoscope.
“Another issue we thought important to address was the availability of voice therapy for patients who are transgender or have a voice that does not match their gender identity,” says Dr. Rameau, who with her Weill Cornell Medicine colleagues created Attuned, a free voice and speech coaching iOS app made for the transgender community to support individuals in their exploration and attainment of a voice that matches their gender identity. Funded by the Dean’s Diversity and Healthcare Disparity Research Awards through Weill Cornell Medicine in 2019, the project is a result of the collaboration of speech pathologists and laryngologists at NewYork-Presbyterian/Weill Cornell, along with members of the transgender community.
Subsequently, Dr. Rameau with colleagues at Stony Brook University conducted a retrospective consecutive case series of 16 transgender women enrolled in a 12-week gender-affirming voice and communication modification program. Self-reported outcomes and changes in acoustic measures of the voice were found to not always correlate.
“Voice therapy for people transitioning genders is not widely available in the country,” says Dr. Rameau. “Unfortunately, there are a lot of ways that people try to change and modify their voice that is not necessarily healthy. It’s not just a matter of the fundamental frequency or the pitch. There are also components such as resonance, prosody or the pace at which you speak, and also vocabulary. With our app, we offer a comprehensive curriculum with highly detailed videos and exercises that train the user and help them to achieve the gender identity they want to reach with their voice.”