Over the last decade, Philip De Jager, MD, PhD, deputy director of the Taub Institute for Research on Alzheimer’s Disease and the Aging Brain at NewYork-Presbyterian and Columbia, has pursued investigations into the genes and proteins involved in mechanisms that contribute to cognitive aging and dementia.
In his most recent research, published in Nature, Dr. De Jager and his team employed single-cell technologies to analyze the brain tissue samples from deceased older adults. Their research identified specific cell subtypes that play a role in the progression of Alzheimer’s, with compelling findings on the cellular changes that occur in the early stages of the disease.
Below, Dr. De Jager discusses the study’s findings and implications for clinical therapeutics.
Research Background & Methods
The brain has a complex architecture with many different cell types, all of which interact with one another. While past studies have analyzed brain samples as a whole, they did not provide any cellular detail. However, we now have single cell technologies to look at the brain in finer resolution at the level of individual cells.
In our study, we constructed a comprehensive cell atlas of the aged frontal cortex of the human brain from individual profiles of 1.65 million brain cells sampled from 437 older individuals participating in the Religious Orders Study or the Memory and Aging Project based at Rush University. The participants enter the studies non-demented and undergo annual cognitive testing until they pass away and their brains are collected.
Our atlas defined 96 different cell subtypes in these brain samples, and we deployed advanced statistical methods to address three challenges:
- We wanted to identify those cell subtypes that are involved in Alzheimer’s disease.
- We wanted to understand how these cells communicate with one another.
- Given the fact that cognitive decline is caused by many different processes, we wanted to identify the subset of participants who were on a trajectory to developing Alzheimer’s disease vs. another dementing process.
We identified two trajectories of brain aging, one of which leads to Alzheimer’s disease and the other path leads to a less understood form of alternative brain aging.
— Dr. Philip De Jager
Key Findings
Using a data-driven approach, we were able to use these cellular profiles to understand the dynamics of the brain’s cellular environment with advancing age. We identified two trajectories of brain aging, one of which leads to Alzheimer’s disease and the other path leads to a less understood form of alternative brain aging.
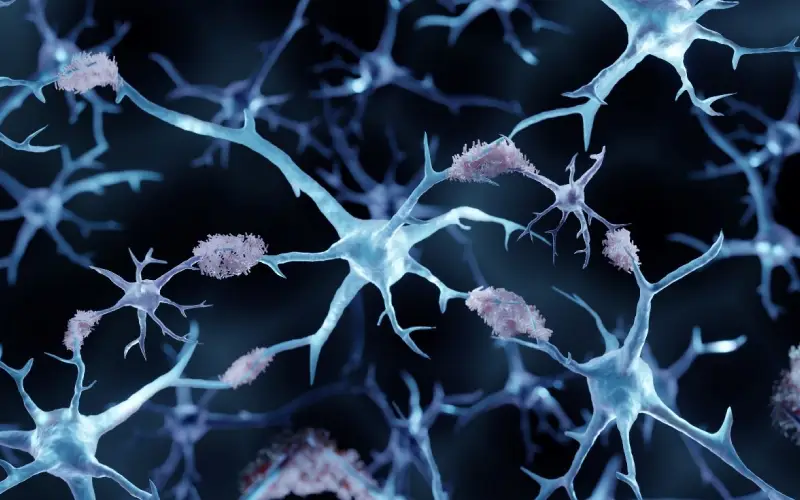
Looking more closely at the path leading to Alzheimer’s disease with advanced statistical modeling, we proposed that two different types of microglial cells, the resident immune cells of the brain, begin the process of amyloid and tau pathology accumulation that defines Alzheimer’s disease. After these pathologies have accumulated, astrocytes, the support cells of the brain, then play a key role in altering electrical connectivity in the brain that leads to cognitive impairment. These microglial and astrocytic cells communicate with each other and bring in additional cell types that lead to a profound disruption in the way the human brain functions with advancing age.
Microglial cells begin the process of amyloid and tau pathology accumulation that defines Alzheimer’s disease.
Microglia, in general, only comprise about 5% of brain cells and, within the microglia, only 1% of these cells are of this pathologic subtype. It’s a tiny number but plays a significant and outsized role. The same is true for the pathologic astrocytes. This makes sense as Alzheimer’s disease is a slowly evolving disease: a small number of cells can perturb cognitive networks over time.
By identifying the sequence of changes in cells involved in Alzheimer’s and distinguishing these changes from those associated with normal brain aging, we were able to solve a major challenge in Alzheimer’s research.
— Dr. Philip De Jager
In addition to microglia and astrocytes, other glial cells may also play a role. Ultimately, all of these cells do not work in isolation, they are constantly sensing their environment and communicating with one another. What we found in our data is that Alzheimer’s disease is a disease of many cells and their interactions, not just a single type of dysfunctional cell. By identifying the sequence of changes in cells involved in Alzheimer’s and distinguishing these changes from those associated with normal brain aging, we were able to solve a major challenge in Alzheimer’s research. Now that we know the cell types involved, we can move toward designing personalized therapeutic interventions to block microglia and astrocytes from adopting those pathologic subtypes. Presumably, this may help to prevent the transition from amyloid to tau and then cognitive impairment.
Future Implications
We have moved forward with research to further understand the molecules that are making the cells develop these pathogenic subtypes with the idea of preventing them from differentiating. We need to understand the best way to modify these cellular communities to preserve cognitive function in the subset of individuals who are on the trajectory to Alzheimer’s disease.
We need to understand the best way to modify these cellular communities to preserve cognitive function in the subset of individuals who are on the trajectory to Alzheimer’s disease.
— Dr. Philip De Jager
Currently, we have one therapeutic intervention for Alzheimer’s disease using antibodies against the amyloid protein. It works, but not very well. We may be able to enhance this existing therapeutic, combine it with another agent, or pursue new therapies that attack other parts of the cascade.
The next steps include replicating the results of our study in other datasets, identifying molecules for therapeutic development, and exploring biomarkers in living individuals through spinal fluid and blood samples. Our research also aims to incorporate spatial transcriptomics to capture three-dimensional data and reconstruct how the brain’s rich architecture is altered by Alzheimer pathology.
Our results provide an important new foundation for therapeutic development by highlighting which cells to target in Alzheimer’s disease and which individuals may be the most likely to respond to Alzheimer’s therapies.



