Some patients with severe brain injury who are behaviorally unresponsive, such as those in a coma or a vegetative state, can show brain activation on neuroimaging in response to motor imagery commands. This phenomenon, known as cognitive motor dissociation or hidden consciousness, was previously thought to occur in just 10% to 20% of patients with disorders of consciousness.
But a new study, published in the New England Journal of Medicine and led by Nicholas D. Schiff, MD, a neurologist at NewYork-Presbyterian/Weill Cornell Medicine, suggests that many more people with disorders of consciousness may have undetected brain activity.
Dr. Schiff, who originally coined the term cognitive motor dissociation in 2015, shares the findings from his recent study and discusses how changes are needed in the clinical management of patients with disorders of consciousness.
Research Background
Our work began decades ago at NewYork-Presbyterian with neuroimaging of patients in a vegetative state and grew into a multinational effort that has uncovered that widely connected networks in the brain can be turned on in some patients in minimally conscious and even vegetative states responding to complex task command. Over time, we have developed these methods using functional magnetic resonance imaging (fMRI) and electroencephalography (EEG) to identify such undetected brain activity in patients with disorders of consciousness.
Research Methods
In this most recent study, we asked the question, just how often does this occur? Our prospective cohort study included 353 adults with disorders of consciousness, making it the largest study ever conducted in this patient population. NewYork-Presbyterian and Weill Cornell Medicine was one of six global sites that contributed clinical and behavioral data on patients with disorders of consciousness to the study. We also collected fMRI and EEG data that showed how these patients responded to motor imagery commands over the course of several minutes, such as picturing opening and closing their hands or swimming in a pool.
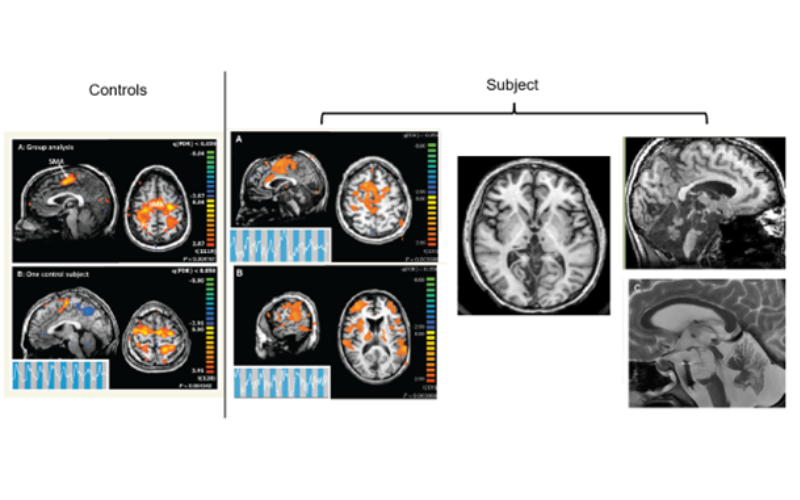
First CMD patient studied at NewYork-Presbyterian and the first independent reproduction of the findings of fMRI-based command following in the scientific literature.
Key Findings
Among the 241 patients who were unresponsive to verbal commands at the bedside, 25% of patients showed brain activity on fMRI, EEG, or both when asked to perform these types of cognitive tasks. Additionally, among the 112 patients who were minimally conscious and had some level of responsiveness, 38% had task-based brain activation on fMRI or EEG.
It is both significant and concerning for a quarter of patients who are not behaviorally responsive to show this type of brain activation. It is concerning because it so often goes undetected, leaving those patients without adequate treatment for their brain injury.
— Dr. Nicholas Schiff
To be able to respond to those imagery commands means that the patient was able to focus attention, hold a task, and be present and allocate cognitive resources. It is both significant and concerning for a quarter of patients who are not behaviorally responsive to show this type of brain activation. It is concerning because it so often goes undetected, leaving those patients without adequate treatment for their brain injury.
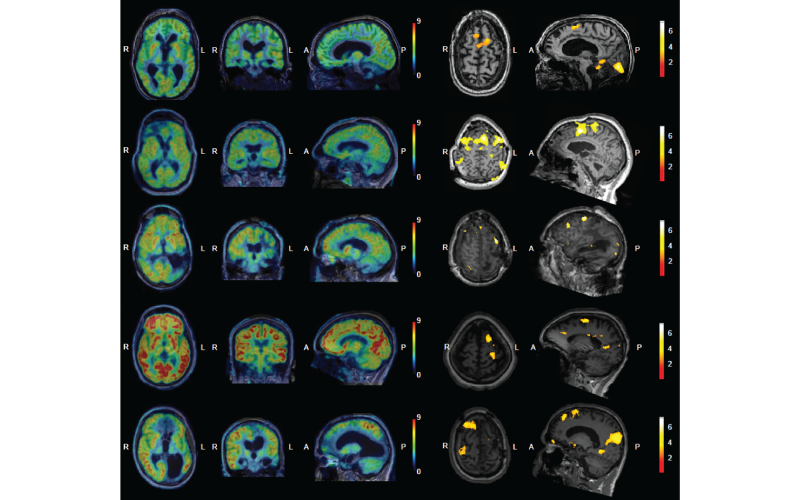
Five additional CMD patients were identified in our own studies among others.
Future Implications
Most patients in a coma, vegetative state, or minimally conscious state do not receive an fMRI or EEG because these modalities are considered research tools, not screening tools. Since they are designated as research tools, they are generally only available at specialized centers like NewYork-Presbyterian and Weill Cornell Medicine, limiting access. Clinical guidelines are split on whether the tools should be used for all patients with disorders of consciousness, in certain cases where there are questions about brain activity, or not at all. Moving forward, we need to validate and standardize fMRI and EEG methods so that cognitive motor dissociation does not continue to go unrecognized.
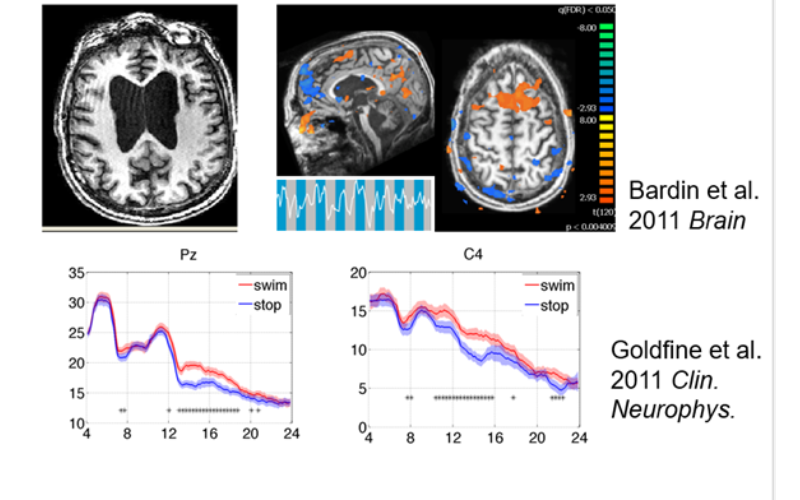
The correspondence between fMRI and EEG-based analyses for one of the patients.
I am optimistic that these findings will help us uncover ways to communicate with patients who have high levels of cognitive function but lack the motor skills to communicate. Tools already exist to help patients with speech and motor disabilities to communicate, such as eye tracking technology. Now that we know that a significant portion of patients with disorders of consciousness also have cognitive function, we can begin to harness the existing brain-computer interfaces to help these patients reach the outside world again.
More than anything, these findings should change the way we view patients who are diagnosed with a coma or in a minimally conscious state. We need to start asking why patients aren’t responsive and what we can do about it, not simply ignoring them. At NewYork-Presbyterian and Weill Cornell Medicine, we have been working on ways to leverage deep brain stimulation and invasive neurological devices to begin the process of helping these patients communicate and potentially take the first step on their road to recovery.



