Mobile Stroke Units Increase Odds of Averting Stroke
Oct 26, 2023
New York, NY
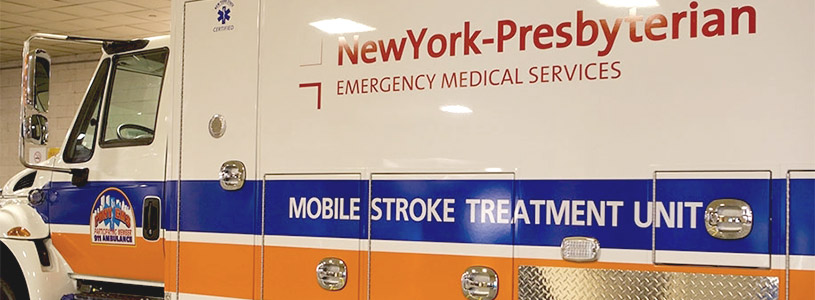
Receiving a clot-busting drug in an ambulance-based mobile stroke unit (MSU) increases the likelihood of averting strokes and complete recovery compared with standard hospital emergency care, according to researchers at Weill Cornell Medicine, NewYork-Presbyterian, UTHealth Houston, Memorial Hermann-Texas Medical Center and five other medical centers across the United States.
The study, published online in the Annals of Neurology on Oct. 6, determined that MSU care was associated with both increased odds of averting stroke compared with hospital emergency medical service (EMS) – 18 percent versus 11 percent, respectively – and a higher percentage of patients – 31 percent versus 21 percent – had early symptom resolution, within 24 hours after stroke.
Patients in this study were treated with tissue plasminogen activator (t-PA), a mainstay medication delivered intravenously (IV) in stroke cases. The drug dissolves the clot in an artery that is blocking blood flow to the brain, making treatment time critical. “While this is known to improve patient outcomes, how many patients fully recover afterward wasn't clear from prior research,” said lead author Dr. Babak Benjamin Navi, associate professor, vice chair for hospital neurology services and chief of stroke and hospital neurology, in the neurology department at Weill Cornell Medicine. He is also acting medical director of the MSU, operated by NewYork-Presbyterian, in collaboration with Weill Cornell Medicine, Columbia University Irving Medical Center, and the Fire Department of New York.
Every Minute Counts When Treating Stroke
“On average, the faster you treat someone, the more likely you are to have a good functional outcome because you’re able to preserve more brain tissue,” Dr. Navi said, who is also associate professor of neuroscience at the Feil Family Brain and Mind Research Institute at Weill Cornell and the medical director of the stroke center at NewYork-Presbyterian/Weill Cornell Medical Center. “The brain can only sustain reduced blood flow for so long before permanent injury develops.”
Using multicenter trial data from 2014-2020, the researchers evaluated 1,009 patients: 644 received t-PA in an MSU, and 365 received EMS care. Overall, patients received t-PA at a median interval of 87 minutes after the onset of stroke symptoms. The study found that with t-PA treatment in this time frame, about one in four patients who had a suspected stroke recovered within 24 hours and one in six averted a stroke with no demonstrable trace of brain injury on an MRI.
The outcome improved for patients treated by an MSU since the time from symptom onset to treatment was 37 minutes faster than for EMS care, meaning many more patients received vital t-PA within the crucial first hour. MSU care further increased the odds of averting a stroke with nearly one-third of patients recovering to normal within 24 hours. In addition, the researchers found other factors that contributed to better patient outcome: treatment within the first 45 minutes, younger age, being female, history of high cholesterol, lower blood pressure, lower stroke severity and no blockage of large blood vessels.
Bringing the Treatment to the Patient
Every 40 seconds, someone in the United States has a stroke, according to the American Heart Association. This study highlights the need for optimizing stroke systems of care, Dr. Navi said. Further expediting the delivery of t-PA through MSUs should be a priority to increase the proportion of averted strokes.
Dr. Navi is also hoping that Medicare will assign MSU services a billing code in the near future so that it can be embedded within stroke systems of care and become a financially viable model.
Currently, he is working with researchers from UTHealth Houston on a study to evaluate the cost effectiveness of MSUs, which should be published next year. “Such studies will hopefully lead to a shift in regulations and reimbursements, and how MSUs are led, managed and integrated within emergency medical services,” he said.
Co-principal investigators for the BEST-MSU trial, which produced the data for this analysis, were Dr. James C. Grotta, director of stroke research at the Clinical Innovation and Research Institute at Memorial Hermann - Texas Medical Center and director of the Mobile Stroke Unit Consortium; and Dr. Jose-Miguel Yamal, department of biostatistics at UTHealth Houston School of Public Health.
This study was funded by grant R-1511-33024 from the Patient-Centered Outcomes Research Institute.
Many Weill Cornell Medicine physicians and scientists maintain relationships and collaborate with external organizations to foster scientific innovation and provide expert guidance. The institution makes these disclosures public to ensure transparency. For this information, see the profiles for Dr. Babak Benjamin Navi.
— Courtesy Weill Cornell Medicine newsroom
Media Contact:
Office of Communications [email protected]


