Cardio-Oncology: Staying Ahead of Cancer Care and Its Cardiovascular Consequences
Managing Malignant Tumors of the Heart
Malignant cardiac tumors are rare and those that metastasize to the heart are much more common than primary cardiac tumors. At NewYork-Presbyterian Hospital, cardiac surgeons join with cardiologists and oncologists in programs dedicated to managing these potentially life-threatening conditions, which could necessitate surgical resection depending on the extent of cardiac structures involved.
An upcoming issue of Advances in Cardiology and Heart Surgery will focus on how Columbia University and Weill Cornell Medicine faculty are addressing these challenging cancers with innovative imaging, novel surgical techniques, and the latest medical therapies.
For more information on our cardiac tumor cancer programs, visit Columbia University and Weill Cornell Medicine.
In the rapidly evolving field of cardio-oncology, NewYork-Presbyterian Hospital is making its mark with dedicated programs led by cardiology faculty at Columbia University Vagelos College of Physicians and Surgeons and Weill Cornell Medicine. The programs leverage the expertise of premier academic departments in cardiology, cardiac surgery, oncology, and imaging, united in a mission to address the adverse effects of cancer therapies on the heart – a major cause of morbidity and mortality in oncologic populations.
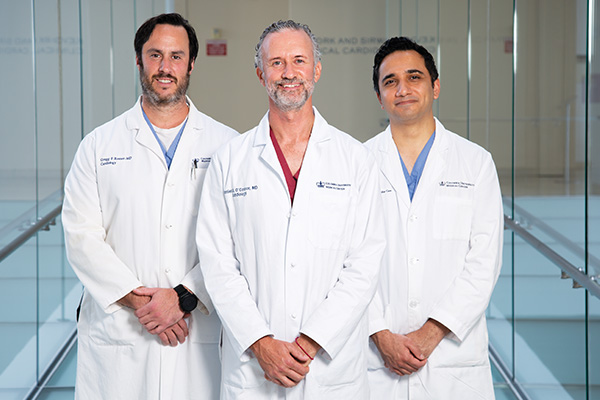
Daniel S. O'Connor, MD, PhD, Gregg F. Rosner, MD, and Jayant K. Raikhelkar, MD, are spearheading the Center for CardioOncology at NewYork-Presbyterian/Columbia University Irving Medical Center; Syed S. Mahmood, MD, MPH, is a physician-scientist with the cardio-oncology program at NewYork-Presbyterian/Weill Cornell Medical Center.
A Cardiology-Oncology Alliance
Dr. Gregg F. Rosner, Dr. Daniel S. O'Connor, and Dr. Jayant K. Raikhelkar
The Center for CardioOncology at NewYork-Presbyterian/Columbia was established in 2009 to meet a clinical need to provide cardiac care to patients undergoing or about to undergo cancer treatment. “This program began as a clinical niche involving cardiologists comfortable providing care to oncology patients,” says Dr. O’Connor, a cardiac intensivist who received his PhD in vascular and cancer cell biology within the Department of Pharmacology at Yale University. “Our objective was to identify individuals at high risk for developing cardio toxic effects of existing and blossoming cancer drugs. The program has since progressed to include a broader purpose with a systems approach that institutes protocols for standards of care and monitoring for different types of cancer.”
Dr. O'Connor and Dr. Rosner, the Center’s Co-Directors, launched the new initiative in collaboration with the breast oncology group at NewYork-Presbyterian/Columbia. “We developed consensus on protocols to identify which patients about to undergo chemotherapy would be considered high risk for cardiac issues and therefore referred for cardiac evaluation and ongoing monitoring for early-onset or late-onset cardiac toxicities,” says Dr. O’Connor.
That first cross-departmental collaboration led to new relationships with multiple myeloma and bone marrow/stem cell transplantation teams and an adult survivors of childhood cancer group. “Early on, most of the adult patients we were seeing were survivors of childhood cancers with lymphoma…individuals who had undergone radiation therapy in the ‘80s and ‘90s,” adds Dr. Rosner. “We also saw many younger patients with Ewing sarcoma who had been treated with high dose anthracyclines.”
“Since establishing the Center for CardioOncolgy, there have been monumental breakthroughs in cancer treatment and, consequently, greater cardiac complications,” continues Dr. Rosner, who also specializes in critical care cardiology and non-invasive cardiac imaging. “Our program continues to adapt its mission and collaborations to keep pace with emerging demands of the field.”
Today, the Center for CardioOncology incorporates the following three-pronged approach:
Collaborating on Clinical Pathways
“We are establishing clinical pathways tailored to each cancer patient based on their particular cancer diagnosis and type of cancer therapy,” explains Dr. Raikhelkar, who completed a clinical/research fellowship in cardio-oncology at Memorial Sloan Kettering Cancer Center and is also a specialist in advanced heart failure and transplant cardiology. “This involves screening patients to identify cardio toxicities as soon as possible, prevent the adverse effects from occurring or progressing, and manage the complications to enable patients to achieve the best outcomes possible. We began by constructing algorithms for the cancers treated commonly with cardiotoxic cancer therapies using a multi-modality approach, including assessment of cardiovascular risk factors, cardiac biomarkers, and use of strain imaging and cardiac MRI when necessary.”
The first clinical pathway developed by the team focused on sarcoma in collaboration with Gary K. Schwartz, MD, Chief of Hematology and Oncology at Columbia, with subsequent protocols created in concert with Dawn L. Hershman, MD, Director of Breast Oncology. The team is currently working similarly with Columbia’s immunotherapy group.
“Sarcoma patients are exposed to the highest cumulative dosage of anthracyclines and we have been able to detect cardiotoxicity earlier in these patients,” says Dr. Raikhelkar. “With the breast oncology group, we modified that protocol to the toxicities that are seen with targeted agents such as trastuzumab for metastatic breast cancer, as well as those patients who receive anthracyclines. We are continuing in this manner to develop unique protocols to make sure we are not only diagnosing heart problems, but also establishing clinical pathways that enhance care and foster communication between the oncology groups and ourselves.”
“We also collaborate with our colleagues in structural heart disease and interventional cardiology,” adds Dr. O’Connor. “While the days of high-dose mediastinal radiation are behind us, the population of people receiving that in their late teenage years to early adulthood is now in the decade of their life where they are experiencing the effects of complex proximal coronary disease and now need bypass surgery or an interventional procedure. These include those requiring TAVR who cannot undergo traditional surgery because of calcific aortas.”
Facilitating Cardio-Oncology Research
“Many programs will not consider heart transplantation in select patients with active cancer,” says Dr. Raikhelkar. “In a survey we conducted in over 50 centers in the United States regarding localized prostate cancer, we found that an overwhelming majority, about 84 percent, are not offering heart transplantation for these patients despite an excellent prognosis with regards to their indolent cancer."
The Center for CardioOncology has accumulated one of the largest experiences in treating cancer survivors who have advanced heart failure with left ventricular assist devices and heart transplantation. The Columbia faculty are studying the outcomes of patients with active cancer undergoing these advanced therapies with a goal to expand them to select individuals who previously have been excluded and may benefit from advanced therapies.
NewYork-Presbyterian/Columbia was one of only 12 tertiary centers in the country to participate in MADIT-CHIC, a multicenter study to determine if cardiac resynchronization therapy (CRT) with a defibrillator or pacemaker in patients with chemotherapy-induced cardiomyopathy (CHIC) can improve left ventricular ejection fraction without adversely affecting mortality. The preliminary study sought to add to the scant data available on the benefit of CRT for patients with CHIC. The findings in the 26-patient cohort based on follow-up data at 6 months showed that the mean left ventricular ejection fraction changed from 28 percent to 39 percent, a statistically significant difference indicating that CRT was associated with major improvement in left ventricular function.
Promoting Awareness
The Center’s mission also addresses the need for education related to new cancer therapies and their potential for heart-related toxicities. “The developments are so rapid in the field that we are all working to educate other physicians as new information comes to light,” notes Dr. Raikhelkar. “It is imperative that physicians in internal medicine, general cardiology and heart failure, and oncology play a role in communicating evidence-based guidance on cancer patients at high risk for developing heart disease.” On October 7, 2021, the Division of Cardiology at NewYok-Prebyterian/Columbia will host its inaugural Cardio-Oncology Summit.
Reference Article
Raikhelkar J, Pham M, Lourenco L, Narang N, Chung B, Nguyen A, Kim G, Sayer G, Uriel N. Heart transplantation in patients with localized prostate cancer—Are we denying a life-saving therapy due to an indolent tumor? Clinical Transplantation. 2020 Nov;34(11):e14080.
Understanding Cardiac Toxicities of Novel Cancer Therapies
Dr. Syed S. Mahmood
“As a cardio-oncologist, it is my goal to help cancer patients tolerate cardiac side effects of life-prolonging cancer therapy and to optimize the heart health of cancer survivors,” says Syed S. Mahmood, MD, MPH, a physician-investigator at the cardio-oncology program at NewYork-Presbyterian/Weill Cornell. “The field of cardio-oncology dates back to the 1960s when anthracycline cancer therapy was first introduced. Early on cardiologists noted dose-dependent cardiac toxicity, which led to the reduction in the dosing of anthracycline. The field has continued to advance, maturing into its own subspecialty within cardiology over the last several years.”
The NewYork-Presbyterian/Weill Cornell cardio-oncology program brings together the world-class research and clinical expertise of oncologists and cardiologists, including subspecialists in cardiac imaging, heart failure, electrophysiology, and interventional cardiology. The program centers on supporting cancer patients so they may complete their oncological therapy while treating cancer therapy related toxicities such as heart failure, myocarditis, or arrhythmias.
Cancer Immunotherapy and the Heart
With immunotherapy now one of the most promising areas of cancer treatment, understanding its cardiotoxicity – particularly those involving immune checkpoint inhibitors and chimeric antigen receptor T-cells (CAR-T) – has become an important focus of cardio-oncologists. Since his subspecialty fellowship in cardio-oncology at Massachusetts General Hospital, Harvard Medical School, Dr. Mahmood helped create one of the largest international registries of cardiotoxicity associated with immune checkpoint inhibitors and CAR-T cancer therapies. That cardiotoxicity, says Dr. Mahmood, includes fulminant myocarditis and heart failure. The work of Dr. Mahmood has been funded by grant support from the New York Academy of Medicine and has greatly expanded the understanding of this cancer immunotherapy related toxicity.
Dr. Mahmood explains that because immune checkpoint inhibitors essentially hyper-activate T-cells to attack the cancer cells, they can also cause autoimmunity in organ systems. “This can result in a high occurrence of toxicity on the liver, in muscles, on the endocrine system, and on the heart, of which myocarditis is perhaps the most deadly.”
“With the expected widespread use of immune checkpoint inhibitors not only as end-of-the-line cancer therapy, but also as an adjuvant cancer therapy, more and more of our patients will be administered this otherwise life-prolonging cancer therapy,” notes Dr. Mahmood. “Our research suggests the estimated occurrence of myocarditis in these patients ranges up to 1 percent. With data from our international registry, we were able to describe the clinical course of patients with myocarditis after receiving immune checkpoint inhibitors. In addition, we showed that troponin levels beyond a certain cutoff are particularly associated with major adverse cardiovascular events, including cardiogenic shock and mortality in up to half of this population. The study also demonstrated the benefit of treatment of this cardiotoxicity with high dose steroids.”
Similarly, CAR-T therapy treats cancers once thought incurable by genetically modifying T-cells to target cancer. Dr. Mahmood’s research has shown that CAR-T recipients are at risk for developing heart failure or arrhythmias due to the inflammatory milieu generated by this T-cell therapy. Together with his colleagues, he has also shown that early use of anti-cytokine agents reduces the cardiotoxicity rate and helps patients tolerate this breakthrough immunotherapy.
Cardiac Imaging to Risk Stratify for Cancer Therapy Toxicity
Research has demonstrated that advanced imaging modalities such as cardiac MRI and echocardiography speckle tracking strain allow for identifying cardio-oncology patients at risk for cancer therapy related cardiotoxicity. Data from an international study looking at CMR across 23 sites, including NewYork-Presbyterian/Weill Cornell, has shown that cardiac MRI based T1 mapping and application of the modified Lake Louise Criteria provides important diagnostic as well as prognostic value in immune checkpoint inhibitors myocarditis patients.
Similarly, using echocardiographic speckle tracking assessment, Dr. Mahmood and colleagues across the country and internationally demonstrated in a multicenter study that reduced global longitudinal strain predicts occurrence of major adverse cardiovascular events. “We found that global longitudinal strain, which is a sensitive biomarker of cardiac toxicity among patients receiving standard chemotherapy, decreases with immune checkpoint inhibitor-myocarditis and, compared with control subjects, was lower and strongly associated with major adverse cardiac events among cases presenting with either a preserved or reduced ejection fraction,” notes Dr. Mahmood. “These are the patients you have to be very careful about and give high dose steroids. We can now risk-stratify these patients early on in their presentation and identify who is going to get so sick that you need to increase immune suppression to try and save their life.”
Novel Treatment of Cancer Immunotherapy Toxicity
While corticosteroids are the first-line treatment for myocarditis, guidelines related to timing, dosage, and treatment strategies vary significantly. With a fatality rate of up to 50 percent in patients undergoing immunotherapy with an immune checkpoint inhibitor who develop myocarditis, the need to identify and standardize optimal treatment strategies is critical.
Again calling on the international registry, Dr. Mahmood and researchers across the multiple sites undertook a retrospective observational study on treatment with corticosteroids to determine when and how much to administer to optimize outcomes. “The study showed a dose dependent effect exists in that the higher the dose of steroids, the more successful the treatment,” says Dr. Mahmood. “In addition, we demonstrated that immune checkpoint inhibitor myocarditis should be considered equivalent to acute coronary syndrome. We found that the longer you wait to initiate lifesaving steroid therapy to turn off the T-cells that the checkpoint inhibitor has hyper-activated, the higher the mortality. If you suspect the patient has ICI-myocarditis, it’s an emergency that has to be acted on immediately.”
Reference Articles
Thavendiranathan P, Zhang L, Zafar A, Drobni ZD, Mahmood SS, et al. Myocardial T1 and T2 Mapping by Magnetic Resonance in Patients With Immune Checkpoint Inhibitor-Associated Myocarditis. Journal of the American College of Cardiology. 2021 Mar 30;77(12):1503-1516.
Zhang L, Zlotoff DA, Awadalla M, Mahmood SS, et al. Major Adverse Cardiovascular Events and the Timing and Dose of Corticosteroids in Immune Checkpoint Inhibitor-Associated Myocarditis. Circulation. 2020 Jun 16;141(24):2031-2034.
Zhang L, Awadalla M, Mahmood SS, et al. Cardiovascular magnetic resonance in immune checkpoint inhibitor-associated myocarditis. European Heart Journal. 2020 May 7;41(18):1733-1743.
Awadalla M, Mahmood SS, et al. Global Longitudinal Strain and Cardiac Events in Patients With Immune Checkpoint Inhibitor-Related Myocarditis. Journal of the American College of Cardiology. 2020 Feb 11;75(5):467-478.
Alvi RM, Frigault MJ, Fradley MG, Jain MD, Mahmood SS et al. Cardiovascular events among adults treated with chimeric antigen receptor T-cells (CAR-T). Journal of the American College of Cardiology, 74(25), 3099-3108.
Mahmood SS, et al. Myocarditis in Patients Treated With Immune Checkpoint Inhibitors. Journal of the American College of Cardiology. 2018 Apr 24;71(16):1755-1764.