Merging Surgical Expertise to Uproot Cardiac Sarcomas

Dr. Leonard N. Girardi and Dr. Jeffrey L. Port
As a group, cardiac tumors affect less than one percent of the population, and most of the tumors are benign. Within this population, however, 25 percent of these tumors are malignant, and of those, 75 percent are sarcomas. This potentially lethal and rare type of primary malignant tumor generally starts in the muscle or blood vessels of the heart. Survival depends on the extent of cardiac structures involved and if surgical resection – considered the definitive treatment for cardiac sarcomas – is even possible. With medical therapy alone, the prognosis is dismal.
“There are two broad categories of cardiac tumors – primary cardiac tumors and other tumors within the chest that invade the heart or great vessels,” says Leonard N. Girardi, MD, Cardiothoracic Surgeon-in-Chief at NewYork-Presbyterian/Weill Cornell Medical Center.
“Lung cancers, too, can invade cardiac and major vascular structures in the chest such as the aorta and the left atrium. These tumors were previously considered unresectable, and patients were told they should go home and get their affairs in order.”
“Cardiac sarcomas were previously considered unresectable, and patients were told they should go home and get their affairs in order.” — Dr. Leonard N. Girardi
But not at Weill Cornell, where Dr. Girardi and his team of cardiac and thoracic surgeons have demonstrated time and time again that by combining their expertise in the OR they can successfully and completely remove the tumor.
“Often patients are referred to a tertiary center such as NewYork-Presbyterian/Weill Cornell after they have been identified with a cardiac tumor at their local hospital,” notes Jeffrey L. Port, MD, a specialist in thoracic oncology who trained in thoracic surgery at both Weill Cornell and Memorial Sloan Kettering Cancer Center. Dr. Port’s practice is largely focused on the surgical treatment of lung and esophageal cancers, and tumors of the chest. “The patient generally will have had a cardiac workup for chest pain, shortness of breath, or blood clots and then a tumor is found coming from a major vessel of the heart or from the lung and has begun growing into the heart, or it can be a metastasis that ends up in or around the major vessels of the heart.”
Aligning Surgical Skill Sets
Working closely with cardiovascular surgeons Mario F. Guadino, MD, and Christopher Lau, MD, and thoracic surgeons Nasser K. Altorki, MD, Division Chief, Thoracic Surgery, and Brendon M. Stiles, MD, Dr. Girardi and Dr. Port take a combined approach to address tumors that invade the heart.
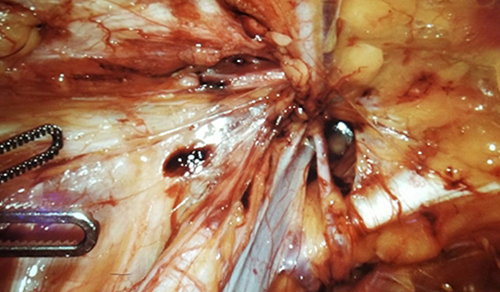
“Between cardiac and thoracic surgeons, we are able to resect these tumors, reconstruct sections of the heart, and replace a valve or a portion of the heart,” says Dr. Girardi. “We’ve done a very good job of taking on patients who sometimes need major cardiac or great vessel resection and reconstruction in order to get them cancer free. Because some of the tumors are unresponsive to chemotherapy or radiation therapy, many of these patients are looking for solutions to an unsolvable problem. As a result, patients come to us from all over the country. We can give these patients a new lease on life.”
“As thoracic surgeons, we are called upon to work with our cardiac surgeon partners in the joint task of going after a malignancy that crosses into the heart or emanates from the heart,” adds Dr. Port. “This requires a combination of our skills to free the tumor from the heart, from the lung, and from the surrounding structures. These surgeries are technically challenging and ultimately require the resources of both specialties. They are complex operations that take the better part of the day. Many of these tumors will require a patient to be put on a heart-lung machine while we work to take the cancer out of the roots of the heart, if you will.”
“As thoracic surgeons, we are called upon to work with our cardiac surgeon partners in the joint task of going after a malignancy that crosses into the heart or emanates from the heart.” — Dr. Jeffrey L. Port
With two surgical teams in place, Dr. Port notes that they often do as much of the operation as possible without putting the patient on blood thinners. “During the last part of the surgery when the patient has to be placed on the heart-lung machine and be fully anticoagulated, Dr. Girardi and I work together,” says Dr. Port. “If there is a defect in the heart and the muscle of the chamber, he will reconstruct that portion and I remove the rest of the tumor. Then together we manage the care of the patient in the postoperative setting. It definitely requires a team approach and is dependent on the talents of both teams. This approach does not exist in many cancer centers, which do not have heart surgeons or bypass capabilities, or services for patients with existing cardiac disease or previous bypasses. We can also provide the intensive care support and full service care found at a university hospital.”
“As long as we are able to get negative margins, which is crucial, patients do very, very well,” says Dr. Girardi. “The way to achieve this is with experience and with aggressive surgery. Compared to a lung or colon cancer where you can achieve a 2, 3, 4, 5 cm margin or the optimal margin that current guidelines recommend, you can’t do that in the heart. We are looking for microscopically and physically grossly negative margins otherwise the recurrence rates are much higher and survival is not very good. So you must get negative margins. For example, if the pulmonary artery is involved, the patient may need to have a pneumonectomy. If that’s what it takes to get microscopically margin-negative results, you do it.”
In the April 2019 issue of The Annals of Thoracic Surgery, Weill Cornell faculty report on their 20-year experience with180 patients who underwent resection of benign or malignant cardiac tumors, with a specific focus on cardiac sarcomas. Sixty-one of the patients had malignant tumors, and 10 of these patients had primary cardiac tumors all of which were sarcomas. The authors note, “With cardiac sarcomas, particular thought must be given to operative planning and timing because the optimal method to improve survival is a complete resection on the first attempt.” The authors also note that neoadjuvant therapy is now known to increases the rate of complete resection and therefore improve survival.
Reference Article
Lau C, Leonard JR, Schwann AN, Soletti G, Abouarab AA, Munjal M, Gaudino M, Girardi LN. A 20-Year experience with resection of primary cardiac tumors and metastatic tumors of the heart. The Annals of Thoracic Surgery. 2019 Apr;107(4):1126-1131. https://www.annalsthoracicsurgery.org/article/S0003-4975(18)31673-4/fulltext#figures
Related Publications
A Novel Shunt Approach Shows Promise for End-Stage Pulmonary Arterial Hypertension