The Upward Trajectory of Robotic-Assisted Radical Cystectomy
Douglas S. Scherr, MD
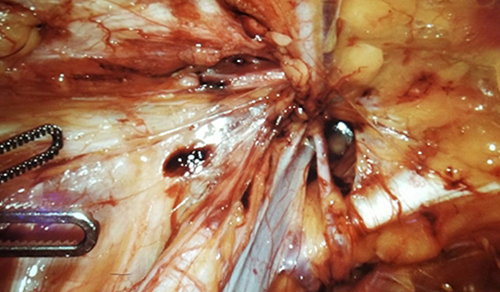
Robotic-assisted radical cystectomy has assumed its rightful place in the skill set of urologic oncologists. The application of robotics to perform radical cystectomy has been steadily increasing since its introduction nearly two decades ago. Urologic oncologists in the Department of Urology at NewYork-Presbyterian/Weill Cornell Medical Center were among the earliest adopters of the procedure and, having accumulated unparalleled experience in the field, continue to refine the techniques and technology that address the morbidities of open surgery.
In a comprehensive review of robotic radical cystectomy in today’s management of bladder cancer, Douglas S. Scherr, MD, Clinical Director of Urologic Oncology, and Weill Cornell Medicine urologic faculty detail the many aspects of the approach – from patient selection to oncologic outcomes – that facilitate its success in treating patients with bladder cancer.
Latitude in Patient Selection
Studies have shown that no major differences exist in evaluating patients for either robotic or open procedures for radical cystectomy, although consensus guidelines include a number of co-morbidities that should be considered in decision-making. These include obesity, extravesical disease, previous vascular surgery, or preexisting cardiopulmonary disease that could be affected by positioning.
Shorter Hospital Stays
Robotic procedures are associated with hospitalizations 2.5 days shorter than open surgery. Although not validated, this shorter length of stay may be related to a number of factors, including the increasing adoption of ERAS protocols, using a minimally invasive approach, fewer perioperative transfusions, and proficiency of the surgeon.
Comparable and Favorable Outcomes
Both robotic and open surgery have been shown to have similar oncologic outcomes in terms of time to recurrence, cancer-specific survival, and overall survival. Additionally, a recent meta-analysis in randomized and nonrandomized comparative studies found that complication rates between the two approaches within 90 days were also comparable. Postoperative quality-of-life scores were analogous at 3 and 6 months post-procedure. The general consensus remains that robotic procedures result in significantly less blood loss, with nearly all trials that have included blood loss data indicating an average decrease of approximately 400 mL of blood loss compared with open surgery.
Experience Counts
In general, there is consensus among experts that experience level is an important factor in reaching an acceptable degree of competence. It is recommended that surgeons perform their first 20 to 30 robotic-assisted ileal conduit reconstructions and first 100 robotic-assisted neobladder or continent reconstruction cases under the supervision of an experienced mentor to be considered a proficient robotic surgeon.
Read More
Cai PY, Khan AI, Shoag JE, Scherr DS. Robotic radical cystectomy in the contemporary management of bladder cancer. The Urologic Clinics of North America. 2021 Feb;48(1):45-50.
Related Publications